Have you ever undergone a sleep study or been diagnosed with a sleep disorder? If so, you might be wondering “how often do sleep studies need to be repeated”?
The significance of sleep studies (polysomnography) cannot be overstated when it comes to identifying and managing sleep disorders, enhancing sleep quality, and mitigating health problems linked to sleep disorders.
This article offers a comprehensive analysis of the frequency of sleep studies while also providing tips on preparing for one. Additionally, we will explore the reasons why repeat studies may be necessary and how they can provide essential information on changes and effective treatments.
Frequency of Sleep Studies: How Often Should You Repeat A Sleep Study
In general, sleep medicine experts, like Dr. Sharad Pandhi, recommends a repeat sleep study after the initial treatment to assess the effectiveness of the intervention and then periodically after that to monitor any changes in the condition. The frequency of repeat sleep studies can vary depending on the individual’s condition and treatment plan.
Therefore, the individual’s needs and response to treatment should be the basis of the specified interval for repeat sleep studies.
Every 1-3 Years For Mild to Moderate Sleep Disorders
For mild to moderate sleep disorders, sleep studies are recommended less frequently than for more severe sleep disorders because the risk of complications or changes in the condition is generally lower.
Mild to moderate sleep disorders may respond more to initial treatment and require less monitoring than more severe conditions.
Individuals with mild to moderate sleep disorders may also have less complex sleep-related issues, making it possible for them to manage their symptoms with lifestyle changes or non-invasive interventions, reducing the need for frequent monitoring with sleep studies.
Every 1-2 Years for Severe Sleep Disorders
Severe sleep disorders can significantly affect a person’s health and daily life, such as obstructive sleep apnea, narcolepsy, and severe insomnia.
Sleep medicine experts generally recommend more frequent repeating sleep studies for individuals with severe sleep disorders –– typically ranging from every few months to every year or two, depending on the individual’s condition and treatment plan.
This increased frequency is due to the more significant impact that severe sleep disorders can have on an individual’s overall health and the need for more intensive treatment and monitoring.
In addition, those with severe sleep disorders may have more complex sleep-related issues and require more frequent adjustments to their treatment plan to achieve optimal results.
Reasons to Repeat Sleep Studies

Repeating sleep studies provide valuable information on changes and help identify effective treatments. Here are some of the reasons why you may need a repeat sleep study:
Changes in Sleep Patterns or Symptoms
Insomnia or Hypersomnia
Insomnia or hypersomnia is a sleep disorder characterized by difficulty falling asleep, staying asleep, or waking up too early. Causes include stress, anxiety, depression, medical conditions, and medications, while the common symptoms are:
- Fatigue
- Mood disturbances
- Difficulty concentrating
Snoring or Sleep Apnea
Snoring or sleep apnea is when the airway becomes partially or fully blocked during sleep, leading to loud snoring or pauses in breathing. This causes sleep disturbance, fatigue, and other health problems.
Obesity, aging, and anatomical abnormalities are common causes.
Restless Legs Syndrome or Periodic Limb Movement Disorder
Restless legs syndrome is a neurological disorder distinguished by an uncontrollable desire to move the legs, often accompanied by uncomfortable limb sensations. On the other hand, periodic limb movement disorder is related to involuntary twitching or jerking movements during sleep.
The causes of these disorders are not fully understood, but genetics and underlying medical conditions may play a role.
Nightmares or Sleepwalking
Nightmares and sleepwalking are two parasomnias that occur during sleep; sleep studies can help identify these conditions.
Nightmares are vivid, disturbing dreams that can cause intense fear, anxiety, or sadness. At the same time, sleepwalking involves getting out of bed and walking or performing other activities while still asleep, often with no memory of the event afterward.
The causes of nightmares and sleepwalking can vary and may be related to underlying health conditions, medication use, or psychological factors.
Changes in Lifestyle or Health Status
Weight Gain or Loss
Weight gain increases the risk of developing sleep apnea, characterized by symptoms such as snoring, choking, and gasping during sleep. In contrast, weight loss can lead to changes in sleep patterns and the effectiveness of sleep apnea treatment.
Pregnancy
Pregnancy significantly impacts sleep quality due to hormonal changes, physical discomfort, and frequent urination, leading to the development or worsening of sleep disorders, such as insomnia, snoring, or sleep apnea.
Menopause
During menopause, hormonal changes can lead to hot flashes, night sweats, and insomnia, significantly impacting sleep quality.
Chronic illness or Injury
Chronic illness or injury can affect sleep quality and lead to developing or worsening sleep disorders due to pain, discomfort, or medication side effects that can disrupt sleep.
Also, certain sleep conditions like obstructive sleep apnea or periodic limb movement disorder may be more prevalent in those with chronic illnesses or injuries.
Changes in Medications or Treatments
Introduction or Discontinuation of Medications
Some medications, such as antidepressants, steroids, and beta-blockers, cause insomnia, which may lead to a sleep disorder. Conversely, discontinuing certain medications, such as benzodiazepines (commonly prescribed for anxiety), can lead to rebound insomnia.
Changes in Medication Dosages
Increasing the dosage of certain medications used to treat medical conditions such as Parkinson’s disease, depression, or chronic pain leads to side effects that interfere with sleep.
On the other hand, decreasing the dosage of medications used to treat sleep disorders like restless leg syndrome or periodic limb movement disorder can worsen symptoms and disrupt sleep.
Evaluating the Effectiveness of Previous Treatments
Periodic monitoring can help identify changes in sleep patterns and the development of new sleep disorders.
By assessing the effectiveness of prior treatments, sleep experts can adjust treatment plans accordingly and provide the most appropriate care for their patients.
Determining if treatment goals have been met
Repeat sleep studies can help assess whether a treatment has successfully achieved these goals and if further adjustments to the treatment plan are necessary. For example, in the case of sleep apnea, treatment aims to reduce the number of apneic events that occur during sleep.
By repeating a sleep study after treatment, Dr. Pandhi can evaluate whether the treatment has effectively reduced the number of apneic events and achieved the treatment goal.
Similarly, in the case of insomnia, treatment may lessen the time it takes to fall asleep and increase total sleep time.
Assessing the need for further treatment
To ensure you receive the most effective care possible, repeat sleep studies help identify the need for further treatment by providing valuable information about the nature and severity of these symptoms, allowing healthcare professionals to develop an appropriate treatment plan.
For example, if you have sleep apnea and continue to experience symptoms despite initial treatment with a continuous positive airway pressure (CPAP) machine, repeat sleep studies may be used to assess the need for alternative treatment options such as oral appliances or surgical intervention.
Factors That May Influence the Frequency of Repeat Sleep Studies
Age
As individuals age, their risk for developing sleep disorders increases, which may warrant more frequent repeat sleep studies.
Specifically, sleep medicine experts may recommend more frequent sleep studies for individuals over 60 because they are at higher risk for age-related sleep disorders such as periodic limb movement disorder and sleep apnea.
Severity of Condition
For individuals with severe sleep disorders, sleep medicine experts may recommend more frequent sleep studies to closely monitor the effectiveness of treatment and make any necessary adjustments.
Presence of Comorbidities
Comorbidities, like anxiety, depression, and chronic pain, can impact sleep quality and may require adjustments to treatment plans, resulting in an increased frequency of repeat sleep studies.
Use of Medications or Other Treatments
The frequency of repeat sleep studies for individuals using medications or other treatments will depend on the specific treatment and individual response.
Preparation for Repeat Sleep Studies
Avoid Caffeine, Nicotine, and Alcohol Before the Test
Avoid consuming caffeine, nicotine, and alcohol for at least 24 hours before the sleep study to ensure accurate results and reduce the risk of interfering with the sleep test.
Follow Your Normal Sleep Routine
Taking a nap or sleeping in can disrupt your natural sleep cycle, making falling asleep during the test more difficult. It can also affect the quality and quantity of sleep you get during the trial, which can compromise the accuracy of the results.
So, following your regular sleep routine is critical to prepare for a sleep study because it helps ensure accurate results by providing a baseline for your typical sleep patterns and habits.
Bring Comfortable Sleepwear and Personal Hygiene Items
Bring comfortable sleepwear, such as loose-fitting clothing made of breathable fabric, and personal hygiene items, such as a toothbrush, toothpaste, and any necessary medications to ensure comfort and proper hygiene during the sleep study.
Notify the Sleep Technologist of Any Discomfort or Problems During the Test
Any pain or problems you experience can affect your sleep, leading to inaccurate results. The technologist can address these issues, such as adjusting the electrodes or providing additional support or equipment.
Follow Up With Your Healthcare Provider After the Test to Discuss the Results
By working closely with your healthcare provider, you can ensure that the sleep study results are accurately interpreted and that any necessary interventions are implemented to improve your overall sleep health.
What to Expect During the Sleep Study
During a sleep study, you will spend the night in a private room designed to simulate a comfortable bedroom environment while being monitored by a sleep specialist to diagnose any potential sleep disorders or issues.
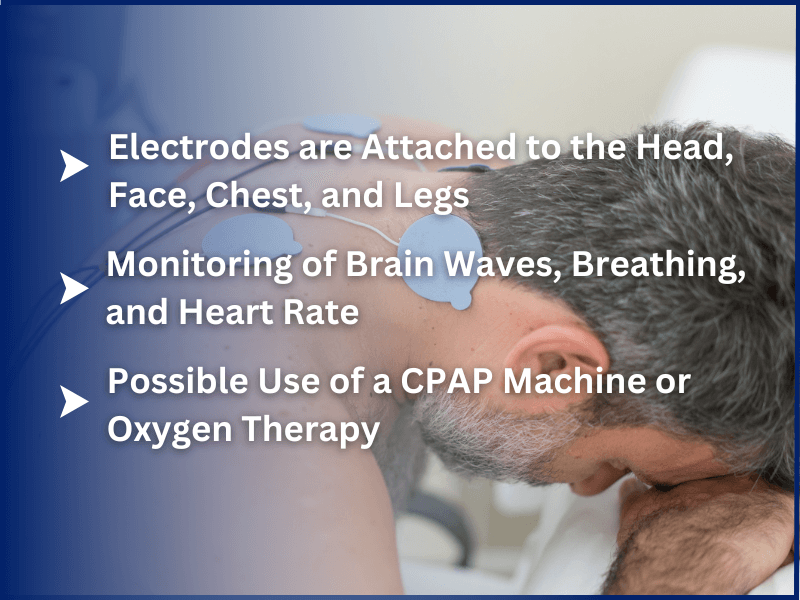
Electrodes are Attached to the Head, Face, Chest, and Legs
You will be hooked to various sensors, including electrodes attached to the head, face, chest, and legs, to monitor brain waves, eye movement, muscle activity, heart rate, and breathing patterns while you sleep.
Monitoring of Brain Waves, Breathing, and Heart Rate
The sleep specialist will monitor your brain waves, breathing, and heart rate using an Electroencephalography (EEG), which will be attached to your head, face, and chest, respectively.
Breathing is monitored using nasal airflow sensors and belts around the chest and abdomen to measure respiratory effort, while your heart rate is measured using ECG with electrodes placed on the chest.
Possible Use of a CPAP Machine or Oxygen Therapy
A Continuous Positive Airway Pressure (CPAP) machine may be used during a sleep study if you have been diagnosed with sleep apnea –– a condition characterized by pauses in breathing during sleep.
The CPAP machine delivers continuous air pressure to keep the airway open and prevent interruptions in breathing.
Final Words
Repeat sleep studies may be necessary to monitor the effectiveness of treatment for sleep disorders or to assess changes in sleep patterns over time.
These steps can help ensure that the sleep study results are accurate and effective in improving sleep health.
If you’re experiencing difficulty sleeping or suspect you may have a sleep disorder, contact Sleep Perfection today to schedule a sleep study.
FAQs
Do sleep study results expire?
Sleep study results do not necessarily expire, but their relevance may diminish over time, depending on the nature of the sleep disorder being evaluated.
For instance, if you were diagnosed with a sleep disorder and received treatment based on the results of a sleep study, it may be necessary to repeat the sleep study to assess the effectiveness of the treatment or to monitor changes in your sleep patterns.
Additionally, you have experienced significant changes in your health or lifestyle since your previous sleep study. In that case, a repeat sleep study may be necessary to assess any changes in your sleep quality.
Ultimately, the decision to repeat a sleep study should be made in consultation with your healthcare provider based on your circumstances and needs.
How many sleep studies are performed annually?
It is difficult to provide an exact number of sleep studies performed annually, as it can vary depending on location, population, and the healthcare system.
Nonetheless, as awareness of the importance of sleep health continues to grow, it is expected that the number of sleep studies performed annually will continue to increase in the coming years.
Are sleep studies always accurate?
Various factors, such as anxiety, discomfort, or medication use, can affect the accuracy of the results. Additionally, interpreting the results of a sleep study requires expertise and experience. Therefore, working with a qualified healthcare provider who can accurately decipher the results and develop an appropriate treatment plan is essential.







